Table of Contents
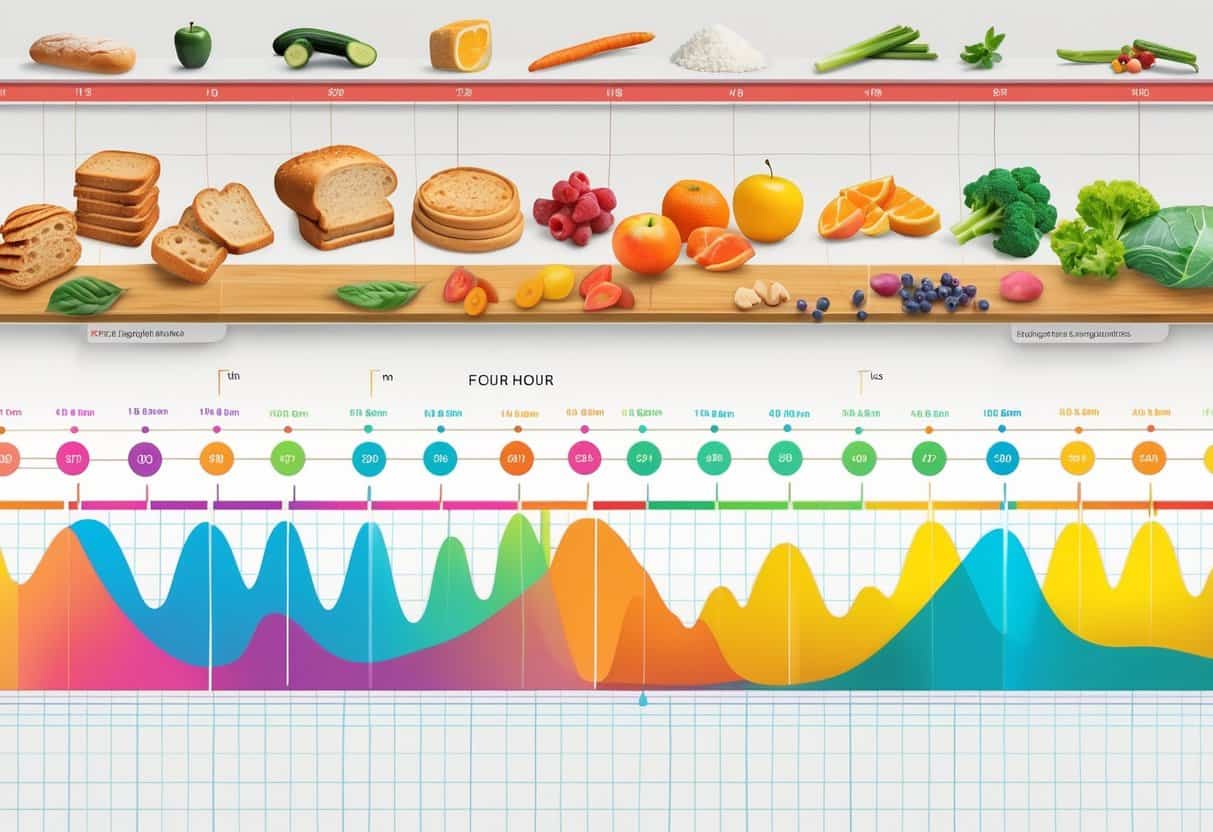
Food changes your blood sugar in real time, often hour by hour after you eat. Usually, blood sugar rises and peaks between one and two hours after a meal, then drops back down within about three hours.
The type of food you eat totally changes how fast and how much your blood sugar shifts.
Carbohydrates create the biggest jumps in blood sugar. Protein and fat slow things down.
If you know how your meals affect your blood sugar through the day, you can manage your energy and health way better. That’s especially true if you’re dealing with diabetes or need to keep an eye on your numbers.
Watching your blood sugar after eating gives you useful feedback. It lets you make smarter food choices and tweak your habits to keep things steady.
Key Takeaways
- Blood sugar usually peaks 1-2 hours after eating, then returns to normal within 3 hours.
- Different foods cause different speeds and levels of blood sugar changes.
- Tracking your blood sugar helps you manage energy and health more effectively.
Understanding Blood Sugar and Glucose Levels
Your body uses glucose as its main energy source. How glucose moves in your blood depends on all kinds of things, especially hormones and the gadgets you use to track your levels.
Knowing what blood sugar is, how insulin works, and what your target levels should be helps you keep things in check.
What Is Blood Sugar?
Blood sugar, or blood glucose, is just the amount of glucose in your bloodstream. Most of it comes from the food you eat—especially carbs like bread, fruit, and sweets.
Your body breaks down these foods into glucose for energy. Glucose levels shift all day.
Before eating, they’re usually at their lowest. After you eat, blood sugar goes up as glucose enters your blood.
The timing and height of that peak really depend on what and how much you ate.
You can measure blood sugar with a meter or a continuous glucose monitor (CGM). These tools help you see your numbers, so you can keep things in a healthy range.
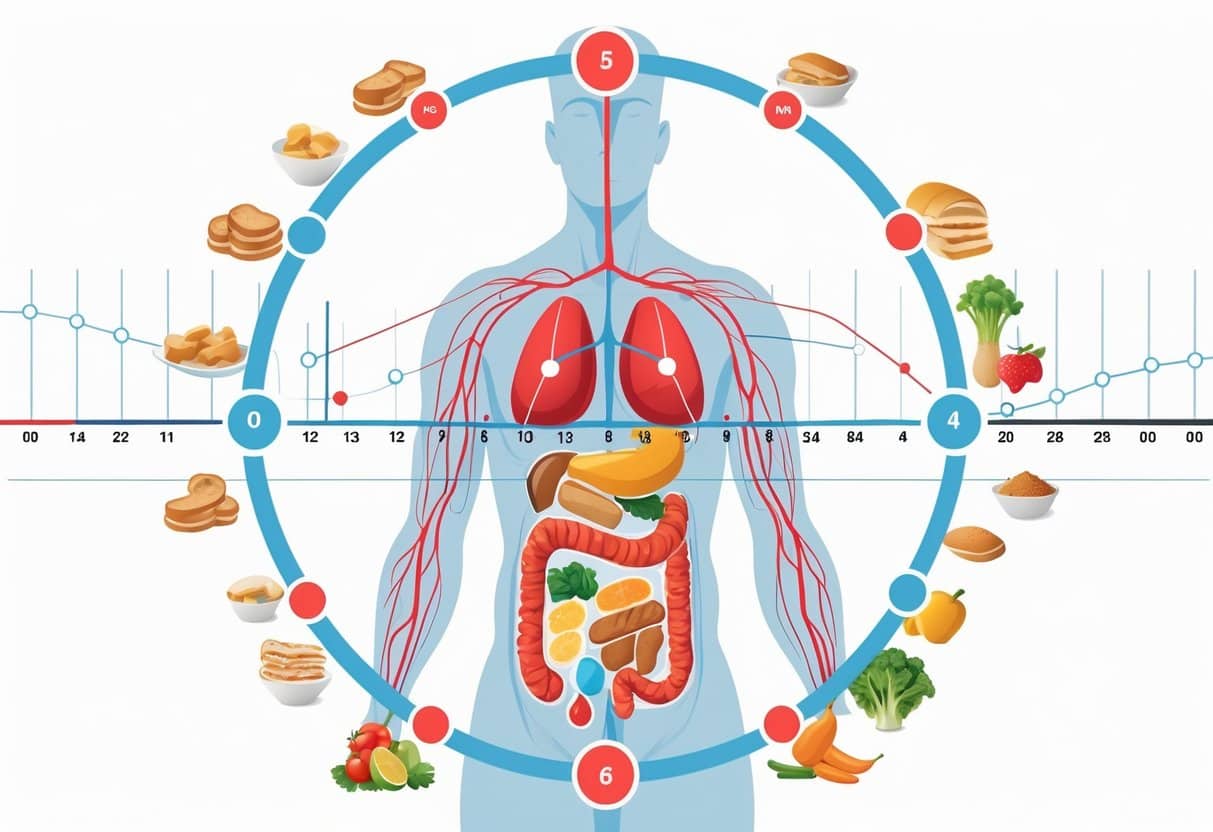
The Role of Glucose and Insulin
Glucose is the fuel your body needs. But it can’t get into your cells by itself—insulin has to help.
Insulin is a hormone from your pancreas. When blood sugar rises after you eat, insulin gets released to move glucose from your blood into your cells.
That’s how your blood sugar drops back to normal. If you don’t make enough insulin or your cells ignore it, glucose builds up in your blood.
That can mean high blood sugar and higher risk for diabetes.
Blood Glucose Targets and Monitoring
There are specific blood glucose targets that help you stay healthy. Before meals, aim for 80 to 130 mg/dL.
Two hours after eating, try to keep blood sugar below 180 mg/dL. Using a meter or CGM lets you check if you’re hitting those targets.
Regular monitoring shows how food, exercise, and medication affect your levels.
Here are common target ranges:
| Time | Target Blood Glucose (mg/dL) |
|---|---|
| Before a meal | 80 – 130 |
| Two hours after eating | Less than 180 |
Keeping track helps you avoid both low and high blood sugar, which is pretty important for your energy and long-term health.
How Food Influences Blood Sugar Hour-by-Hour
What you eat changes your blood sugar at different times after a meal. Your body releases insulin and moves glucose through your bloodstream.
Watching these patterns helps you manage your blood sugar better.
The Immediate Impact of Eating
When you eat, carbs break down into sugar, which hits your bloodstream fast. The more carbs, the quicker your blood sugar rises.
Simple carbs like sugar or white bread cause the quickest spikes. Your body releases insulin to help move sugar from your blood into cells.
If insulin’s doing its job, blood sugar stays in a healthy range. Eating protein or veggies before carbs can slow sugar absorption and reduce those big spikes.
Blood Sugar Patterns in the First Hour
In the first hour after eating, blood sugar often jumps up. How high it goes depends on what you ate and how much insulin your body makes.
Eating late at night can cause higher blood sugar and less insulin response. If your blood sugar is low before a meal, your stomach might empty food faster, making glucose rise even quicker.
Continuous glucose monitors really show this early increase for a lot of people.
Glucose Fluctuations Over Several Hours
After that first spike, blood sugar usually starts to fall as insulin does its thing. This can take 2-3 hours or even longer, depending on what you ate and your metabolism.
Eating late or skipping meals can cause higher average blood sugar. You might see more ups and downs if your insulin response isn’t great.
A glucose monitor helps you spot patterns and adjust when or what you eat to keep things more stable.
| Time After Eating | Typical Blood Sugar Change | Influencing Factors |
|---|---|---|
| 0-30 minutes | Rapid increase from carb digestion | Type and amount of carbs, pre-meal blood sugar |
| 30-60 minutes | Peak blood glucose level | Insulin response, gastric emptying speed |
| 1-3 hours | Gradual decrease as insulin acts | Meal size, food order, insulin sensitivity |
Carbohydrates and Blood Sugar Response
Carbs directly affect your blood sugar by turning into glucose during digestion. The kind of carb you eat changes how fast and how much blood sugar rises.
Knowing the difference between sugary foods and other carbs can help you manage your blood sugar.
Effect of Sugary Foods
Sugary foods have simple sugars that get absorbed into your bloodstream super quickly. This causes a fast spike in blood sugar.
You might feel a quick energy boost, but it’s often followed by a sharp drop—leaving you tired or hungry again.
Sugary foods can be tough to manage, especially if you have diabetes or prediabetes. Eating them in big amounts or on an empty stomach makes blood sugar swings worse.
Combining sugary foods with protein, fiber, or fat can slow digestion and keep blood sugar steadier.
Complex vs. Simple Carbohydrates
Complex carbs have longer chains of sugar molecules, so they take more time to break down. This means a slower, steadier release of glucose.
Whole grains, veggies, and beans are good examples. Simple carbs, like those in candy or soda, break down fast.
Not all simple carbs are terrible—fruits have natural sugars plus fiber, which helps slow things down. Picking complex carbs over simple ones helps you avoid sudden spikes and crashes.
Quick comparison:
| Type | Digestion Speed | Effect on Blood Sugar | Examples |
|---|---|---|---|
| Simple Carbohydrates | Fast | Quick spike | Candy, soda, white bread |
| Complex Carbohydrates | Slow | Steady rise | Oats, beans, vegetables |
Paying attention to the type of carbs you eat can make a real difference in keeping your blood sugar steady.
The Role of Protein and Fat in Glucose Regulation
Protein and fat change how fast carbs break down and enter your bloodstream. They slow down digestion, so blood sugar levels don’t swing as much.
Protein’s Impact on Blood Sugar
Protein doesn’t raise blood sugar nearly as much as carbs. When you eat protein, your body can make some glucose from it, but it happens slowly.
So, protein causes a mild, drawn-out rise in blood sugar. Including protein with meals can help reduce those sharp spikes from carbs.
It also helps you stay full longer, which might cut down on snacking that can raise blood sugar.
How Dietary Fat Alters Glucose Absorption
Fat slows down how fast your stomach empties, so carbs get digested more slowly. That means glucose enters your blood more gradually.
Fat itself doesn’t raise blood sugar directly. But eating a lot of fat over time might mess with how your body uses insulin, making blood sugar control trickier for some.
Adding fats like avocado, nuts, or olive oil to meals can help keep your blood sugar more stable when you eat carbs.
Special Considerations for Diabetes
If you’re managing blood sugar hour-by-hour, you really have to pay attention to how everything affects your numbers. Balancing food, medication, and activity keeps you from going too high or too low.
Type 1 Diabetes and Blood Sugar Management
With type 1 diabetes, your body doesn’t make insulin, so you have to give yourself shots or use a pump. Blood sugar can rise fast after eating carbs, so timing your insulin matters.
Watch for hypoglycemia (low blood sugar), especially before meals and after exercise. Carry fast-acting sugar just in case.
High blood glucose can happen if your insulin dose is too low or your meal has more carbs than you thought.
Check your blood sugar every few hours, especially after meals and before bed.
Type 2 Diabetes: Hour-by-Hour Changes
For type 2 diabetes, your body still makes insulin but doesn’t use it well. Blood sugar changes can be slower, but meals, activity, and stress still affect things.
Carbs have the biggest impact. Eating similar amounts of carbs at regular times helps prevent spikes.
Fat and protein slow digestion, so sugar levels stay steadier longer. You might use medication or insulin—just depends on your doctor’s advice.
Monitor your levels around meals and after exercise to avoid high blood glucose or hypoglycemia.
Diabetic Ketoacidosis Risks
Diabetic ketoacidosis (DKA) happens when your body can’t use sugar for energy and starts breaking down fat, creating dangerous acids called ketones.
You’re at risk if your blood sugar stays really high for hours, especially with type 1 diabetes. Signs include nausea, vomiting, rapid breathing, and confusion.
Check your blood sugar and ketones if you feel sick or your levels are high. DKA is an emergency—don’t wait to get help.
Table: Signs of Low and High Blood Sugar
| Condition | Symptoms | Action Needed |
|---|---|---|
| Hypoglycemia | Shaking, sweating, dizziness | Eat or drink fast sugar |
| High blood sugar | Thirst, frequent urination | Adjust meds, check ketones |
Managing Hyperglycemia and Hypoglycemia
You’ve got to keep an eye on your blood sugar to avoid big highs and lows. Knowing the signs and how to react quickly is key.
Recognizing and Addressing Hyperglycemia
Hyperglycemia means your blood sugar is too high. Signs include thirst, tiredness, blurry vision, and peeing a lot.
If you notice these, check your blood sugar. To lower high blood sugar, drink water to help flush out extra sugar.
Move around a bit if your doctor says it’s okay. Skip carbs until your levels come down.
If your blood sugar stays high or you feel sick, call your health care team. They might need to adjust your medication or insulin.
Preventing and Treating Hypoglycemia
Hypoglycemia is when blood sugar drops below 70 mg/dL. Symptoms are shakiness, sweating, confusion, or weakness.
Always have fast-acting carbs like glucose tablets or juice handy. To treat a low, have 15 grams of simple carbs, wait 15 minutes, and test again.
Repeat if needed. Don’t ignore symptoms, especially if you’re driving or using machinery.
Eat regular meals with a balance of carbs, fat, and protein to help prevent lows. Adjust your meds and activity with your health care team’s advice.
Lifestyle Factors That Influence Blood Sugar Patterns
Your blood sugar shifts all day based on what you eat, how active you are, and when you eat. Habits can make blood sugar rise or fall in different ways.
Fasting and Its Effects
When you fast, your body uses stored energy since you’re not eating. This usually causes blood sugar to drop.
If you fast too long, though, your body might release stored sugar from your liver, causing blood sugar to rise for a bit.
Short fasts between meals can help stabilize blood sugar by cutting down on spikes from frequent eating. But long fasts may raise stress hormones, which can push blood sugar up—especially if you have diabetes.
The effects of fasting really depend on your health, how long you fast, and how often you do it. Keep an eye on your blood sugar during fasting to see how your body responds.
Role of Physical Activity
Physical activity helps your muscles pull sugar from your blood, which lowers blood sugar levels. Exercise can have both immediate and lasting effects on glucose.
After you work out, your body becomes more sensitive to insulin. This helps move sugar from your blood into your cells.
That insulin effect can stick around for several hours, giving you better blood sugar control. It’s kind of amazing how long it lasts, honestly.
Different workouts hit your blood sugar in different ways. Aerobic exercise tends to lower blood sugar more than quick, high-intensity bursts.
If your blood sugar is really high, though, you might want to skip intense workouts. Sometimes, hard exercise can actually push your levels up even more.
Building a Healthy Diet
Carbohydrates have the biggest impact on blood sugar. The body turns them into sugar pretty fast.
Try to eat more complex carbs like whole grains, veggies, and legumes. These raise blood sugar more slowly than white bread or sweets.
Balancing your meals with protein, fat, and fiber can help slow down how fast sugar gets into your blood. Refined sugars and processed foods? Probably best to avoid those, since they spike your levels.
How much and when you eat matters, too. Smaller meals more often can help stop big jumps in blood sugar.
But be careful not to overdo it. It’s a balancing act, for sure.
Pay attention to how different foods affect you. That’s honestly the best way to figure out what keeps your blood sugar steady throughout the day.
Monitoring and Education for Effective Blood Sugar Control
Managing your blood sugar hour-by-hour means tracking your levels and noticing how different things affect you. The right tools, support from your care team, and a bit of education can make a real difference.
Continuous Glucose Monitoring Technologies
Continuous glucose monitors (CGMs) give you real-time blood sugar readings all day. These devices use a tiny sensor under your skin to check glucose in the fluid between your cells.
CGMs can alert you if your blood sugar starts rising or dropping. That way, you can react quickly.
This tech lets you see exactly how food, exercise, and stress change your glucose hour-by-hour. You’ll still need the occasional fingerstick test, but not as often.
You can download CGM data and look over patterns with your health care team. Many people find this feedback super helpful for making food choices or tweaking routines.
Working With Your Health Care Team
Your health care team might include doctors, nurses, dietitians, and diabetes educators. They’re there to help you make sense of your blood sugar data and adjust things like medications or meal plans.
At regular appointments, you can share results from your glucose meter or CGM. Your team can spot patterns—like spikes after meals or dips during exercise.
Got questions about how certain foods might mess with your sugar levels? Don’t be shy—ask away.
They’ll help you figure out amounts, timing, and when to check your blood sugar, especially after eating or being active.
Education and Support Resources
Education really is at the heart of managing blood sugar. The American Diabetes Association has a bunch of resources—think nutrition advice, monitoring guides, and tips for lifestyle tweaks.
There are classes, online tools, and old-school printed guides if that’s more your style. Sometimes just having options makes a difference.
Support groups and diabetes educators? They can be lifesavers. Getting practical tips and a little encouragement goes a long way.
When you know why your blood sugar changes, you start making smarter choices about food. That understanding just feels empowering.
Tracking meals and blood sugar with a log or an app can be surprisingly helpful. It’s not always fun, but it does help you see how your body reacts.