Table of Contents
Your blood sugar level shifts throughout the day, and knowing when it’s too low or too high can really matter for your health.
Shakiness, sweating, hunger, and a racing heartbeat usually point to low blood sugar.
On the flip side, if you feel super thirsty, tired, or need to pee a lot, those could be signs your blood sugar’s too high.
Ignoring these signs? Not a great idea. Checking in with your body and testing your blood sugar regularly can help you catch problems early.
Let’s dig into the key symptoms that might mean your blood sugar’s out of whack.
Key Takeways
- You can spot blood sugar issues by noticing specific physical symptoms.
- Regular monitoring helps you catch things before they get serious.
- Acting quickly on symptoms can keep you safer.
Understanding Blood Sugar Levels
Your body needs a steady supply of sugar in your blood to run properly. This sugar, glucose, gives your cells energy.
The amount of glucose in your blood depends on how your body processes food and how much insulin you have.
What Is Blood Sugar?
Blood sugar is just the amount of glucose floating around in your blood. Glucose mostly comes from carbs in your food.
It travels through your bloodstream to fuel your cells. Your blood sugar goes up and down during the day depending on what you eat and how active you are.
A normal fasting blood sugar is usually under 100 mg/dL. Higher numbers could mean prediabetes or diabetes.
Glucose and Blood Glucose Level
Glucose is the main sugar your body uses for energy. When you eat, your digestive system breaks food down into glucose, which then enters your blood.
Your blood glucose level tells you how much sugar is in your blood at any given moment. Too low—under 70 mg/dL—and you might feel weak, shaky, or dizzy.
When it’s too high, you could feel thirsty, need to pee a lot, or just feel wiped out.
Role of Insulin in Blood Sugar Regulation
Insulin is a hormone your pancreas makes. Its job is to help glucose move from your blood into your cells.
When you eat and your blood sugar rises, insulin steps in to lower it by getting glucose into your cells. If your body doesn’t make enough insulin or can’t use it right, your blood sugar can stay high, which isn’t good over time.
Causes of Low and High Blood Sugar
Blood sugar levels can swing up or down for a bunch of reasons—what you eat, how much you move, and certain health conditions.
Knowing what can cause these swings helps you keep things under control.
Common Causes of Low Blood Sugar
Low blood sugar, or hypoglycemia, usually means your glucose drops below 70 mg/dL. This can happen if you skip meals or eat less than usual, especially carbs.
Physical activity burns up sugar faster, so working out without eating enough or adjusting meds can drop your blood sugar. Drinking alcohol on an empty stomach? That can also lower your sugar.
Taking too much diabetes medicine or insulin is another cause. When your blood sugar drops, you might feel dizzy, shaky, or confused.
Factors Leading to High Blood Sugar
High blood sugar, or hyperglycemia, means there’s too much glucose in your blood. Eating too many carbs or sugary foods is a common reason.
Stress and illness can also push your blood sugar up, since they mess with how your body uses insulin. Skipping your meds or not being active enough lets sugar pile up in your blood.
If you have type 1 or type 2 diabetes, your body might not make enough insulin or use it well, making it harder to keep your sugar steady.
Role of Diabetes and Medicines
If you’re dealing with diabetes, keeping blood sugar in check relies a lot on your meds and daily habits. Diabetes medicines and insulin help your body manage sugar.
Taking too much insulin or diabetes pills can push your blood sugar too low. Missing doses or taking meds late can make it spike.
With type 1 diabetes, your body stops making insulin, so you need to be on top of it. Type 2 means your body doesn’t use insulin well, so lifestyle changes and meds are key.
Checking your blood sugar and adjusting meds based on what you eat or do helps prevent highs and lows.
Warning Signs of Low Blood Sugar
Low blood sugar, or hypoglycemia, brings on a bunch of symptoms. Some are physical, like shakiness and sweating, while others mess with your thinking.
Early Symptoms of Hypoglycemia
When your blood sugar drops below 70 mg/dL, you might feel shaky or suddenly super hungry. Sweating, weakness, and a fast heartbeat are common.
You could also feel anxious, irritable, dizzy, or just plain tired. Tingling lips or a headache sometimes show up too.
Severe Low Blood Sugar Signs
With severe low blood sugar, things get riskier. You might have trouble walking or seeing straight.
Thinking clearly can get tough, and simple tasks feel impossible. In really bad cases, you could have a seizure or pass out.
If you feel weak or act confused, get help fast. Severe hypoglycemia needs quick treatment.
Neurological Symptoms
Low blood sugar hits your brain hard. Confusion, trouble focusing, and feeling just out of it can all happen.
Headaches and slurred speech might show up. If it gets worse, seizures or fainting are possible.
Keep an eye out for changes in how you think or move—those are big warning signs.
Signs Specific to Children and Adults
Kids with low blood sugar can get cranky, cry more, or look unusually tired. They might shake or sweat but can’t always explain what’s wrong.
Adults usually spot early signs like hunger or dizziness. Both kids and adults need quick treatment, but the signs can show up differently.
Warning Signs of High Blood Sugar
High blood sugar shows up when your glucose climbs above normal. It can mess with your day and lead to bigger problems if you don’t catch it.
Common Symptoms of Hyperglycemia
You might get really thirsty and find yourself running to the bathroom more. That’s your kidneys trying to flush out extra sugar.
Other signs? Feeling tired, weak, or having blurry vision. Dry mouth is common, and some people lose weight without trying if their sugar stays high for a while.
If your blood sugar’s above 180 mg/dL, these symptoms get more noticeable.
Long-Term Effects of High Blood Sugar
Letting your blood sugar stay high for too long can do a number on your body. It can damage blood vessels, raising your risk for heart problems or stroke.
Nerve damage is another risk, causing pain or numbness in your hands and feet. High sugar can also mess with your kidneys.
When to Seek Emergency Help
Some high blood sugar signs mean you need help right away. If you feel really weak, confused, or have trouble breathing, call for medical help.
Vomiting, severe stomach pain, or a racing heart are also red flags. These can point to diabetic ketoacidosis—a dangerous condition.
If your sugar’s over 300 mg/dL and you’re not feeling better, don’t wait to see a doctor.
How to Check Blood Sugar Levels
You’ve got a few ways to check your blood sugar—meters, monitors, and lab tests. Each one gives you a different snapshot.
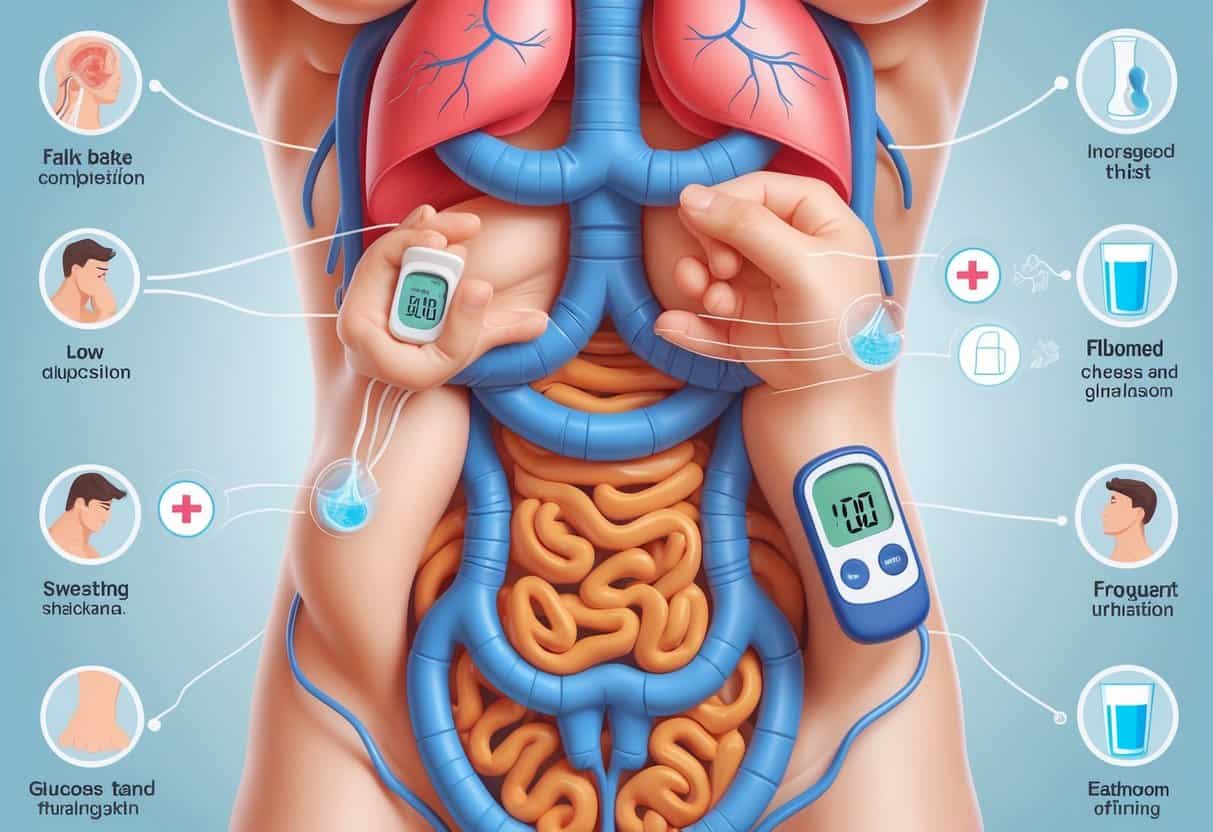
Using a Blood Glucose Meter
A blood glucose meter is a small gadget that tells you your sugar level right then. You need a tiny drop of blood, usually from your finger.
Put the drop on a test strip, and the meter gives you a number in seconds. Don’t forget to wash your hands first.
Checking regularly helps you spot highs and lows. People with diabetes often test several times a day.
Continuous Glucose Monitoring
A continuous glucose monitor (CGM) is a device you stick on your skin. It checks your sugar all day and night by reading the fluid just under your skin.
The CGM sends info to a receiver or your phone, giving you updates every few minutes. You can see trends and get alerts if your sugar goes too high or low.
You might still need to double-check with a meter if things don’t add up.
Blood Tests and Diagnosis
Your doctor can order blood tests for a deeper look. The fasting blood glucose test checks your level after not eating for at least eight hours.
The A1C test shows your average blood sugar over the past couple of months. Doctors use these to diagnose diabetes or prediabetes.
These tests need a lab, so you can’t do them at home.
Treating Low Blood Sugar
When your blood sugar drops, you’ve got to act fast. Fast-acting carbs, like glucose tablets or gel, work for mild cases.
If it’s severe, emergency treatment with glucagon may be needed.
Immediate Actions to Take
If you spot low blood sugar signs, check your level if you can. If it’s under 70 mg/dL, act quickly.
Eat or drink 15 to 20 grams of fast-acting carbs. Some options:
- 4 glucose tablets
- Half a cup (4 ounces) of fruit juice or regular soda
- 1 tablespoon of sugar or honey
Wait about 15 minutes, then check again. If it’s still low, repeat with another 15 to 20 grams.
Avoid eating a ton of food or anything fatty, since that slows down sugar absorption.
Using Glucose Tablets or Gel
Glucose tablets are little sugar pills made to raise your blood sugar fast. They’re easy to carry and have a set amount of glucose.
Take enough tablets to get 15 to 20 grams—usually 3 or 4. They work quicker than candy or juice.
Glucose gel is another option, and you can squeeze it right into your mouth. It’s handy if swallowing is tough.
Keep some tablets or gel with you if you’re at risk for lows.
Glucagon and Emergency Treatment
If you can’t eat or drink, or if you pass out or have a seizure, glucagon is the go-to emergency fix.
A glucagon kit comes as an injection or nasal spray. You need a prescription, and it’s smart to have one if your doctor recommends it.
Someone else can give you the glucagon if you’re not able to. After using it, get medical help right away.
Glucagon tells your liver to dump sugar into your blood fast. It can be a literal lifesaver.
Managing High Blood Sugar
When your blood sugar climbs, you need to bring it down safely. Over time, making changes to your routine helps keep things on track.
Short-Term Management Strategies
If your sugar’s high, check it every few hours. Drink water to stay hydrated.
Skip sugary foods or drinks—they’ll just push your sugar higher. You might need to adjust your meds or insulin, but only with your doctor’s guidance.
Rest if your blood sugar’s really up there, and hold off on hard exercise until it drops.
Keep an eye out for symptoms like frequent urination, extreme thirst, or feeling wiped out. If things aren’t improving after a couple of checks, get in touch with your healthcare team.
Long-Term Blood Sugar Control
Managing blood sugar over time really comes down to juggling your diet, exercise, and any meds you might need. Eat plenty of vegetables, lean protein, and whole grains.
Try to keep carbs in check—they’re the main thing that bumps up your blood sugar.
Getting regular exercise helps your body use insulin better and can lower your blood sugar naturally. Shoot for at least 30 minutes of moderate activity most days.
Keeping a healthy weight makes it easier for your body to manage blood sugar. Talk to your healthcare provider if you need to adjust medication to keep your levels steady.
Lifestyle Strategies for Blood Sugar Balance
Keeping your blood sugar steady is all about daily habits. What you eat, how much you move, and how closely you keep an eye on things really add up.
It’s smart to work with healthcare professionals too—they can help you stay on track.
Dietary Recommendations
Focus on foods that help your blood sugar stay steady. Go for lots of vegetables, fruits, beans, and nuts—they’ve got fiber and nutrients, but won’t spike your sugar.
Try to avoid foods loaded with refined carbs and added sugar. Those can send your blood sugar soaring before you know it.
A good diabetes meal plan mixes protein, healthy fats, and complex carbs. Smaller, regular meals can help keep your blood sugar from crashing.
Don’t forget to stay hydrated—it actually helps with blood sugar stability too.
Skipping meals isn’t a great idea. Try to eat at roughly the same times each day.
This lowers your chances of low blood sugar, especially if you’re on diabetes meds.
Role of Physical Activity
Getting active helps your body use insulin better and brings blood sugar down. Aim for about 30 minutes a day—walking, cycling, swimming, whatever works for you.
If you can’t do it all at once, breaking it up into shorter chunks is totally fine.
Just a heads up: exercise can sometimes drop your blood sugar, especially if you’re on medication. Check your levels before and after, and adjust your food or meds if your doctor says to.
Making exercise a regular thing helps with blood sugar and keeping your weight in a good place.
Monitoring and Prevention
Checking your blood sugar regularly gives you a clearer picture of how your habits affect your levels. Use a glucose meter or a continuous monitor if your provider recommends it.
Watch for signs of both low and high blood sugar. Keeping a log can help you spot patterns.
It’s smart to carry quick sugar fixes like glucose tablets or juice—just in case. Especially if you’re active or your meals get delayed, having a plan for lows is key.
Working With Your Diabetes Care Team
Your diabetes care team—that’s your doctor, dietitian, maybe a nurse—can help you come up with a plan that actually fits your life. They’ll help you figure out what to eat, how to move, and when to tweak things.
They’re also there to guide you if your meds need adjusting or something just feels off. If you notice new symptoms or your routine changes, don’t keep it to yourself.
Let your team know, even if it feels minor. Honestly, it’s worth it—having people in your corner makes managing blood sugar a whole lot less overwhelming.