Table of Contents
Insulin resistance is when your body’s cells just don’t listen to insulin—a hormone that’s supposed to help control blood sugar. This usually leads to higher blood sugar and, eventually, a bigger risk for type 2 diabetes.
Here’s the thing: insulin resistance isn’t set in stone. With some changes to your diet, activity, and maybe your weight, you can actually turn things around.
You don’t have to just live with insulin resistance. By eating fewer processed foods and moving more, you can make your body use insulin better.
These tweaks lower your diabetes risk and just make you feel better overall.
Let’s break down what insulin resistance really is, and what simple things you can try to reverse it.
Key Takeways
- Insulin resistance affects how your body handles blood sugar.
- Lifestyle changes can improve how your body reacts to insulin.
- Early action helps prevent more serious health problems.
Understanding Insulin Resistance
It helps to know how insulin works, what insulin resistance actually means, and how it’s different from insulin sensitivity.
This knowledge makes it easier to see why insulin resistance can mess with your blood sugar and health.
What Is Insulin Resistance
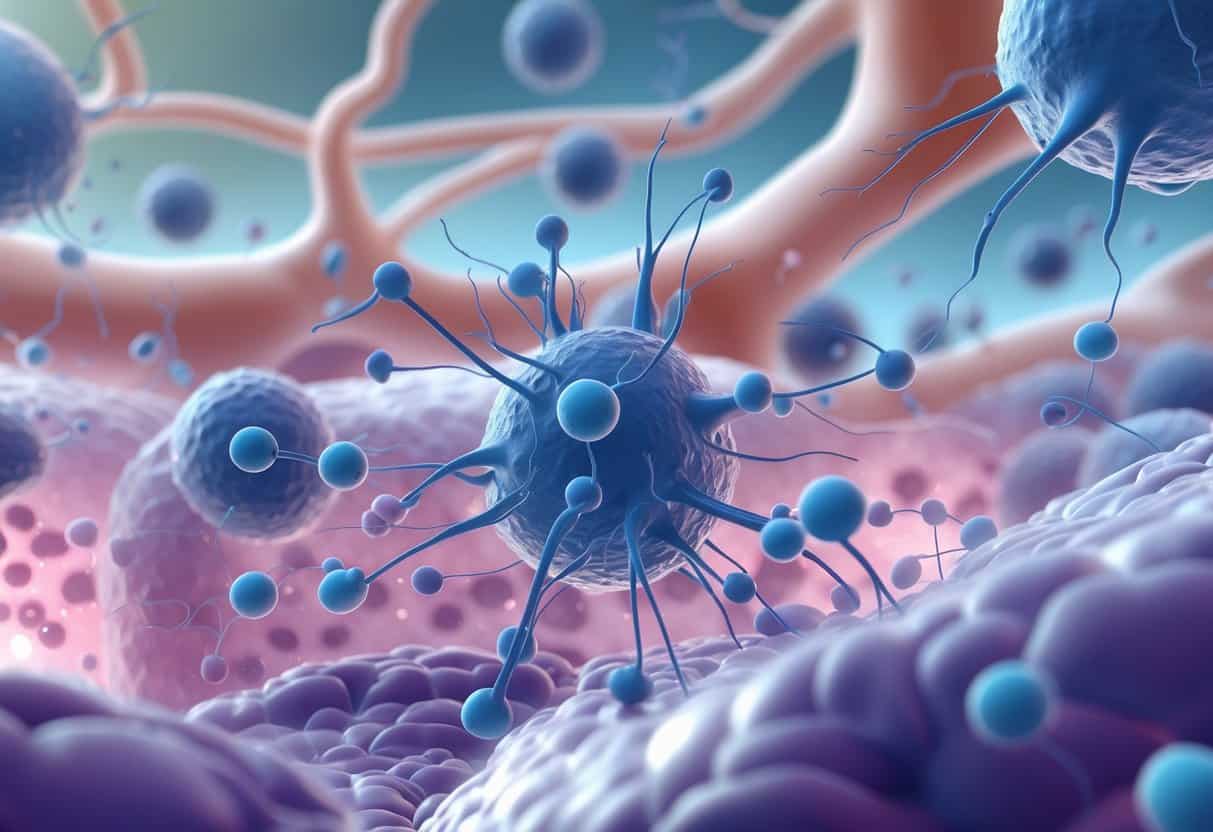
Insulin resistance is when your cells just stop responding to insulin. Insulin, made by your pancreas, tells your muscles, fat, and liver to take glucose out of your blood.
When your cells ignore insulin, glucose piles up in your blood instead of being used for energy.
This can cause high blood sugar. If you leave it alone, your risk for type 2 diabetes and other issues goes up.
How Insulin Works in the Body
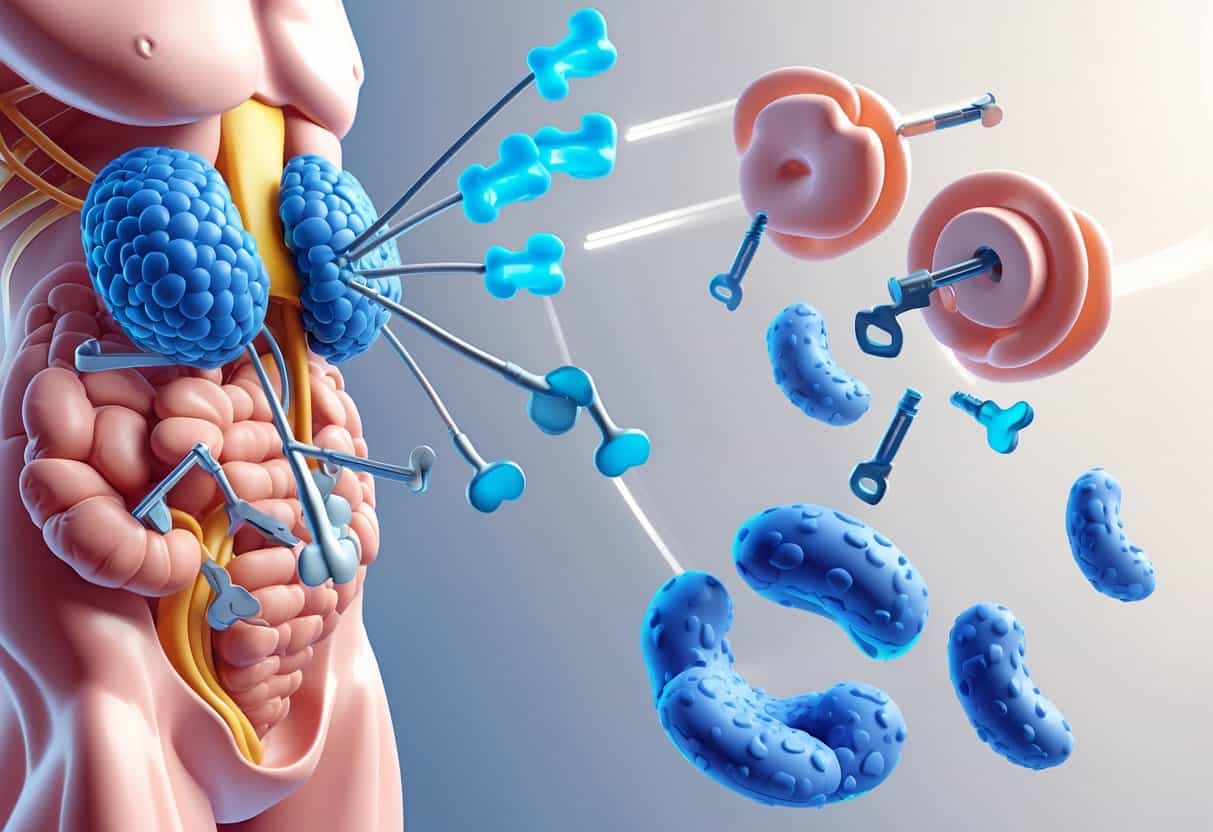
Insulin acts like a key, unlocking your cells so glucose can get in and fuel you. When you eat, your blood sugar rises, signaling your pancreas to release insulin.
That insulin shuttles glucose from your blood into your cells. Your liver grabs some extra glucose and stores it as glycogen for later.
If everything’s working right, insulin keeps your blood sugar in a healthy range.
Insulin Sensitivity vs. Insulin Resistance
Insulin sensitivity means your cells are good at responding to insulin. You don’t need much insulin to keep blood sugar steady.
Insulin resistance is the opposite—your cells ignore insulin, so your pancreas works overtime making even more. Eventually, that can wear your pancreas out.
| Feature | Insulin Sensitivity | Insulin Resistance |
|---|---|---|
| Cell response | Strong | Weak |
| Insulin needed | Less | More |
| Blood sugar control | Good | Poor |
| Risk for diabetes | Lower | Higher |
Causes and Risk Factors for Insulin Resistance
Insulin resistance is basically your body not using insulin well. A bunch of things can play a role—your genes, age, body fat, activity level, and some health problems.
Genetic and Age-Related Factors
Your genes matter here. If close relatives have insulin resistance or type 2 diabetes, your odds go up.
Getting older also makes it harder for your body to use insulin. Even if you’re fit, age can push up your risk.
Some ethnic backgrounds—like African, Hispanic, Native American, and Asian—are more likely to struggle with insulin resistance because of genetics.
Obesity and Body Fat Distribution
Carrying extra weight, especially around your belly, is a big reason people develop insulin resistance. Belly fat (visceral fat) is sneaky—it makes it much harder for your cells to work with insulin.
Waist size is a good clue. More belly fat often means more risk.
This kind of fat actually releases stuff that gets in the way of insulin doing its job.
Physical Inactivity and Lifestyle Influences
Not moving enough is another culprit. Exercise helps your muscles soak up sugar from your blood, making them less insulin resistant.
If you’re not active and your diet’s not great, you’re more likely to gain weight and see your blood sugar creep up.
Even just walking or cycling can help your body handle insulin better. Staying active is honestly one of the easiest ways to lower your risk.
Hormonal and Metabolic Conditions
Some health issues can raise your risk. For example, polycystic ovary syndrome (PCOS) can make it harder for women to use insulin properly.
Other problems like high blood pressure and high cholesterol often show up with insulin resistance and can make things worse.
Hormonal conditions—like Cushing’s syndrome or thyroid issues—can also mess with insulin and blood sugar control.
Symptoms and Health Implications
Insulin resistance changes how your body uses insulin and can bring on a bunch of warning signs. Sometimes, though, the early stuff is so mild you barely notice.
Signs and Symptoms of Insulin Resistance
You might not spot symptoms at first. Common early signs are feeling tired, struggling to lose weight, or just being hungrier than usual.
Some folks get really thirsty or pee more often, which can mean blood sugar is climbing.
A visible clue is darker, thicker skin patches around your neck or armpits—called acanthosis nigricans.
If you’re in the pre-diabetes stage, your blood sugar’s higher than normal, but not quite diabetes-level yet. Often, there aren’t obvious symptoms, but it’s a warning sign.
Associated Metabolic and Vascular Diseases
Insulin resistance can lead to pre-diabetes and, if it keeps going, type 2 diabetes. It also bumps up your risk for things like high blood pressure and cholesterol problems.
It’s not just about blood sugar. You’re more likely to have heart issues, like heart attacks or strokes, because insulin resistance messes with your blood vessels.
Other problems can include gum disease, nerve damage, and even trouble with your eyes or hearing.
Complications and Related Conditions
If insulin resistance isn’t managed, it can cause some serious trouble. It affects blood sugar, fat storage, and blood flow—raising your risk for a bunch of diseases.
Type 2 Diabetes and Blood Sugar Levels
When your cells ignore insulin, they don’t take in sugar well. Blood sugar stays high, and over time, you could end up with type 2 diabetes.
High blood sugar damages organs and nerves. You might notice thirst, tiredness, or peeing a lot.
Diet and exercise really matter here—they help your body respond to insulin and keep blood sugar in check.
Fatty Liver and Nonalcoholic Fatty Liver Disease
Insulin resistance makes it easier for fat to pile up in your liver. If there’s no alcohol involved, it’s called nonalcoholic fatty liver disease (NAFLD).
NAFLD can lead to liver inflammation and, if ignored, even scarring or failure.
You might not feel anything at first. Blood tests or scans can spot fatty liver, though. Losing weight and improving your diet can really help lower your risk.
Heart Disease and Hypertension
Insulin resistance isn’t great for your blood vessels. It raises your chances of heart disease and high blood pressure.
High blood pressure makes your heart work overtime and ups your risk for heart attacks or strokes.
You might not notice symptoms early on. That’s why regular checkups matter. Eating better and moving more both help protect your heart.
Diagnosis and Assessment
Doctors use a few tests to see how your body handles blood sugar and insulin. They’ll also check things like cholesterol to get a full picture.
Testing for Insulin Resistance
The most common tests are fasting insulin and glucose. You’ll probably have to skip breakfast, then get your blood drawn to check those levels.
Another test is the Oral Glucose Tolerance Test (OGTT). You drink something sugary, then get your blood checked a few times over a couple hours.
There’s also the HOMA-IR formula, which uses fasting insulin and glucose numbers to estimate resistance.
Hemoglobin A1c and Blood Glucose Monitoring
Hemoglobin A1c (HbA1c) tells you your average blood sugar over the past few months. It’s a good way to see how things are going long-term.
If you have insulin resistance or prediabetes, regular blood sugar checks at home can help you see what’s working.
An HbA1c between 5.7% and 6.4% means prediabetes—so, kind of a yellow flag. Keeping blood sugar in range lowers your risk for type 2 diabetes.
Cholesterol and Other Biometric Markers
High cholesterol often tags along with insulin resistance. Docs will look at your LDL (bad), HDL (good), and triglycerides.
Insulin resistance usually means higher LDL and triglycerides, and lower HDL. Not a great combo for your heart.
Other measurements—like blood pressure and waist size—are also important since they tend to go hand-in-hand with insulin resistance.
Tracking all these numbers helps your doctor put together a plan that fits you.
Lifestyle Approaches to Reverse Insulin Resistance
You can do a lot to improve insulin resistance by changing up how you eat, move, and manage your weight. These steps help your body use insulin better and keep blood sugar down.
Dietary Strategies for Improved Insulin Sensitivity
Aim for a balanced diet—think lots of veggies, lean protein, and low-fat dairy. These foods don’t spike your blood sugar as much.
Cut back on sugary snacks, refined carbs, and processed stuff. Fiber-rich foods like whole grains, beans, and veggies slow digestion and can help your insulin response.
Don’t go for crash diets—steady, moderate portions are better. A sample day? Maybe grilled chicken, steamed veggies, a bit of brown rice, and fruit for snacks. Oh, and water instead of soda.
Physical Activity and Exercise Benefits
Exercise makes your muscles soak up more glucose and respond better to insulin. Both cardio (like walking or cycling) and resistance training (weights or bands) are good.
Shoot for at least 150 minutes of moderate exercise a week. Strength training a couple times a week helps, too.
Even little things—like taking the stairs or gardening—add up. It all helps your insulin work better.
Weight Management and Weight Loss
Keeping a healthy weight is key. Losing just 5-10% of your body weight can make a big difference.
Weight loss lowers fat in your liver and muscles, making it easier for insulin to do its job. Go for slow, steady progress with a mix of better eating and more movement.
Tracking your progress and setting small goals can help. Building muscle also boosts your metabolism and helps with insulin.
Medical Treatments and Interventions
If lifestyle changes aren’t enough, there are medical options. Some meds can help your body handle insulin or keep blood sugar down.
Pharmacological Treatments
The main drugs are metformin and thiazolidinediones. Metformin makes your liver release less sugar, while thiazolidinediones help your muscle and fat cells respond to insulin.
If you already have diabetes, your doctor might add other meds to control blood sugar or protect your heart.
These medicines don’t cure insulin resistance, but they help manage the problems that come with it. Always follow your doctor’s advice and keep up with healthy habits.
Emerging Therapies and Ongoing Research
Researchers are always hunting for new ways to reverse insulin resistance. Some newer drugs, like GLP-1 receptor agonists, can help by reducing appetite and improving insulin function.
Other studies are looking at ways to lower inflammation or even use gene therapy. Most of this stuff isn’t available yet, but it’s coming.
It’s worth keeping an eye on new developments and talking to your doctor about what’s out there.
Additional Lifestyle Factors
There’s more to insulin resistance than just diet and exercise. Other parts of your lifestyle can make a difference, too. Sometimes, it’s the little things that add up.
The Role of Sleep and Sleep Apnea
Getting enough quality sleep really matters for your insulin sensitivity. Poor or irregular sleep can mess with your hormones, raising your risk of insulin resistance.
Sleep helps keep cortisol and other blood sugar hormones in check. If you’re not sleeping well, those hormones get out of balance.
Sleep apnea, where you stop breathing for short stretches at night, hits your insulin sensitivity too. When your body doesn’t get enough oxygen, stress levels spike, and insulin just doesn’t work as well.
Treating sleep apnea—maybe with a CPAP machine—can help your body respond better to insulin. It’s worth talking to your doctor if you suspect you have sleep apnea.
Aim for 7 to 9 hours of solid sleep each night. Try to keep your bedtime steady, and make your room dark and quiet. These small habits can give your body a real boost in using insulin.
Mental Health and Depression
Depression, unfortunately, can make insulin resistance worse. It’s easy to slip into less activity and poor eating habits when you’re feeling low.
Stress and depression trigger hormones like cortisol, which push blood sugar up and make insulin less effective. It’s a tough cycle.
Managing your mental health is honestly just as important as diet or exercise. If you’re struggling, therapy, medication, or even small lifestyle changes might help.
Relaxation techniques—think meditation or just deep breaths—can support your mental health and help keep those tricky hormones in check.
Prevention and Long-Term Health
Managing insulin resistance isn’t a quick fix. It takes steady attention and a few key lifestyle choices.
Maintaining Long-Term Insulin Sensitivity
To keep insulin working well, staying active is huge. Even a 30-minute walk or bike ride most days can make a difference for your muscles.
Losing a bit of weight, if you need to, can help your body handle insulin better. Go for foods high in fiber, and try to steer clear of refined sugars and processed carbs.
Sugary drinks and snacks like chips? Best to keep those to a minimum.
Sleep and stress matter, too. Shoot for 7 to 9 hours of sleep and try adding stress-busters like meditation or deep breathing into your day. It’s not always easy, but every little bit helps.
Reducing Cancer Risk and Other Complications
Insulin resistance can bump up your chances of getting certain cancers, like breast or colon cancer.
Keeping your blood sugar and insulin levels steady really helps lower these risks.
Lifestyle choices play a huge role here. Eating more veggies, fruits, and whole grains gives your immune system a boost and cuts down on inflammation.
If you can, steer clear of tobacco. Limiting alcohol is wise too—your body will thank you for it.
Regular check-ups make it easier to catch problems early. It’s worth chatting with your doctor about cancer screenings and how to handle other risks, like heart disease or type 2 diabetes.